
Patient experience of dietetic care in New Zealand.
Nutrition is an important aspect of the treatment and management of IBD.
With growing emphasis on dietary therapies in IBD and the need for diet recommendations to be individualised for each person’s circumstances, it is important that dietitians are involved in the multidisciplinary team caring for IBD patients. Anecdotal reports from around New Zealand are that patient access to dietitians is not consistent, although there has been no formal research to assess this.
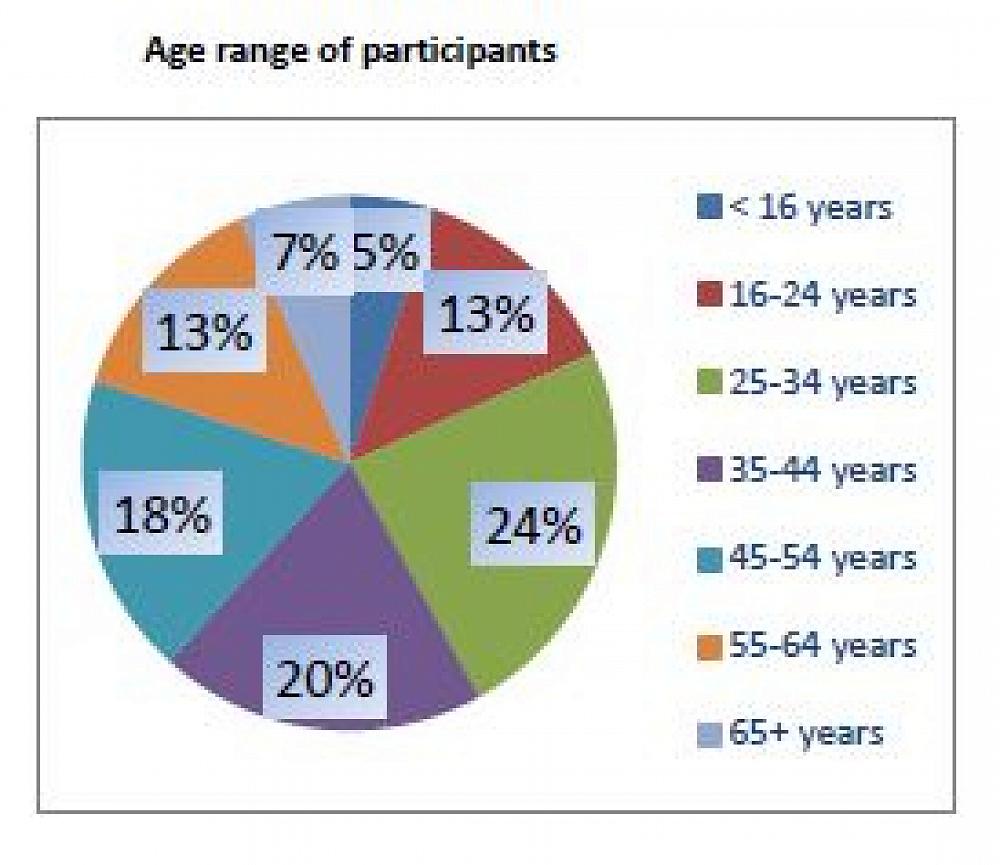
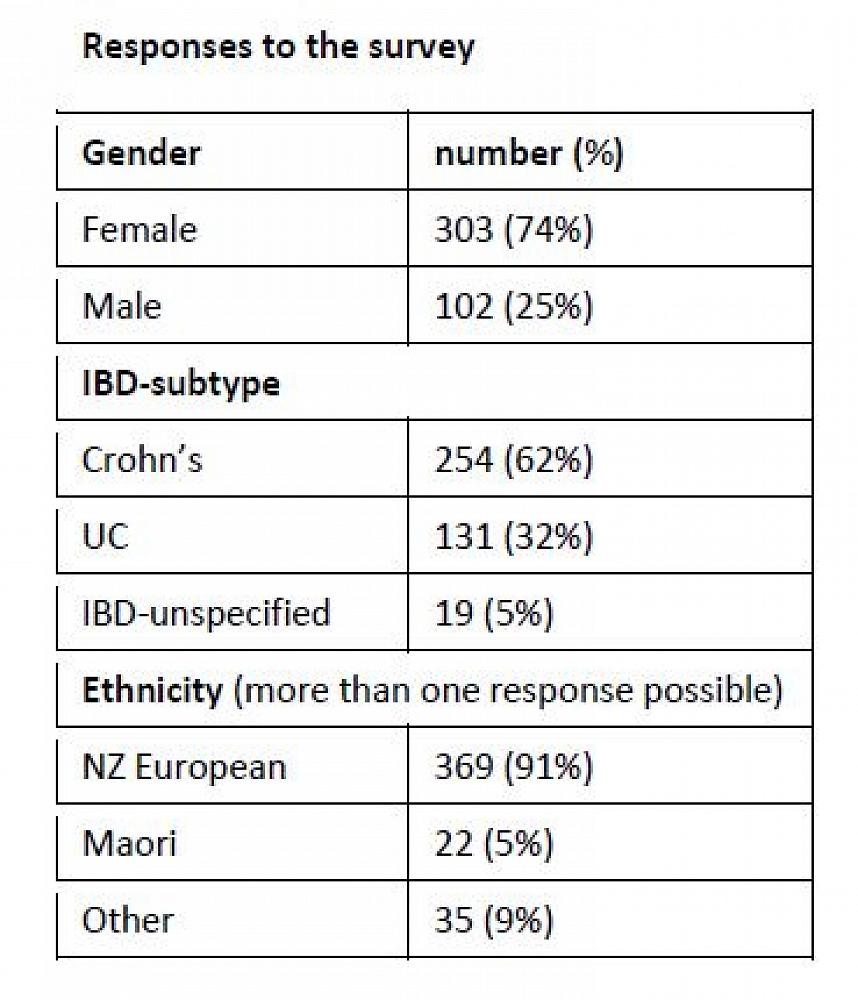
Nicky McCarthy is a dietitian from Central Otago who is researching dietetic care for people with IBD in New Zealand. The research project is supervised by Dr Catherine Wall and Prof Michael Schultz. As part of the project, she sent out a research survey to NZ IBD patients in March/April 2020 to investigate patient experience of dietetic care. Responses are summarized below:
Medications and supplements
Almost all participants (90%) were currently taking at least one medication for IBD and over three- quarters take a supplement of some kind, most commonly vitamins or minerals.

Who has seen a dietitian?
52% of participants had seen a dietitian. Younger participants, those with Crohn’s disease, those currently on biologic therapy and those who had undergone surgery to treat IBD were more likely to have seen a dietitian for IBD advice. There was no link with having seen a dietitian based on a person's gender, ethnicity, years since IBD diagnosis, or travel time to be seen. Over one-third of those who had seen a dietitian paid for their appointment, many because they were ineligible for a publicly funded appointment or unaware that publicly funded services were available.
Views on the role of dietitians in IBD management
In response to the question ‘Do you think it is useful for patients diagnosed with IBD to have access to a dietitian for nutrition advice?’, 349 (86%) responded ‘Yes’ and 49 (12%) responded ‘Maybe’ and 2% (7 people) responded ‘No’.
The majority thought that it would be useful to receive advice immediately or shortly after diagnosis. Two-thirds of respondents thought is would be helpful to see a dietitian anytime new issues with nutrition arose.
Nutrition topics of interest
95% of participants reported at least one IBD nutrition topic that they would like to discuss with a dietitian, with some choosing several topics to discuss.

Other topics suggested included diets to alter gut microbiota, information about vegan diets, foods that worsen IBD symptoms, and how to increase dietary variety.
Type of advice received
The most common type of nutrition intervention/advice received from their dietitian was to follow a particular type of diet (e.g. low FODMAP, low residue etc), general healthy nutrition advice, or prescribing of supplement drinks. Over 90% of participants reported that they followed the dietitian recommendations.
Was the dietitian advice useful?
Participants were asked ‘Was the advice you were given by the dietitian/s useful?’. Participants could choose from the responses: extremely useful, very useful, moderately useful, slightly useful, not at all useful. 66% of respondents found the dietitian advice at least moderately useful. 18% reported that the advice was not at all useful. Those participants who had seen a dietitian in a private clinic or had received written advice were more likely to find the dietitian advice useful.
How to improve services
The final survey question was open-ended to allow participants to give their views on whether improvements are needed to current IBD dietetic services - Do you think that there are any other nutrition or dietitian services that should be offered to IBD patients, or have suggestions for how current services should be improved?
The most common theme in these comments was the need for dietitians to have specific knowledge about IBD and to provide more specific IBD nutrition advice.
‘Have specialist IBD nutritionists available’
‘The first dietitian that I saw really to be fair had no clue but the second one was very good’ ‘Dietitians should be telling me about the latest information.’
Respondents also frequently commented that all patients diagnosed with IBD should routinely be referred to a dietitian and there should be greater access to publicly funded dietitians.
‘I would like to see a routine referral for patients diagnosed with IBD’
‘Nutritional/ dietitian consultations should be part of the process once diagnosis has been made’ ‘I think all people with IBD should see a Dietitian annually alongside blood tests to confirm their nutrition needs are being met as best they can be.’
A common theme was the desire for follow-up from dietitians, so that patients are seen more than once; respondents wished to have dietitians available on an ongoing basis in the same way that IBD nurses were available to answer questions.
‘I would like more regular catchups with a dietitian. I’ve had Crohn’s for 27 years now so would like to see a dietitian to discuss new ideas and nutritional advice.’
‘Better follow up and ongoing diet support’
‘I think MDT specialist appointments with the DT is a great idea. I can contact my gastro nurse via email with questions that don't necessarily require an in-person appointment, the ability to do this with a DT would be really helpful.’
Some respondents had never received dietitian referral even though many reported asking to see a dietitian.
‘As I haven't been offered dietitian services I think being offered that would be a step in the right direction’
‘I have been desperate to see one for years but never had an appointment although I’ve asked many times’
‘I think that every patient should be able to access one for free. I was told that diet has no impact on my IBD at all but would have liked the opportunity to talk to a specialist in that field’
Some respondents took the opportunity to highlight how much they valued the dietetic service they received.
‘Our experience with initial dietician was invaluable’
‘Just want to say my Dietician has been super helpful.’
‘I have been very privileged to have a top class dietician and gastro consultant. We work together as a team.’
Conclusions
It is clear from the survey responses that the demand for dietetic services is greater than what patients are able to access. It appears that there may be barriers to referral, whether this is due to referrer beliefs that patients will not benefit from dietetic input or a lack of available publicly funded services. Equally, the survey indicates that dietitians who are seeing IBD patients would benefit from specialist IBD training.
The next part of this research is to gather information from surveys of gastroenterologists and dietitians to further investigate the issues related to service capacity, service delivery and referral practices. The aim will be to make recommendations for future dietetic service improvement to better meet the needs and expectations of IBD patients.
Acknowledgements
Nicky’s Master of Health Sciences research is supported by Dietitians New Zealand; Rabbitt Education Fund, Dunstan Hospital; Dept of Medicine, University of Otago Dunedin
